
minimal additional surgical injury – this recognises the fact that surgery is an injury.Then, once the bone has healed, usually by 8 weeks, the patient will feel very close to normal The goal is to have regained normal motion in the joints before the bone has healed. early motion – once the bone has been returned to its normal shape and stabilised, it’s time to move! That’s on the day after surgery, for most of my patients.With careful positioning of the implant, the fracture will be stabilised, and the implant “invisible” to the body (see minimising complications). While there are multitudes of implants available, the latest available come with modifications based on the latest understanding of fracture behavior, surgical techniques and complication profiles.The vast majority of distal radius fractures can be stabilised, with the latest plating systems, on the palmar side only. Patients today have the advantage of many previous evolutions of fixation for the distal radius. stable fixation – this means using special titanium implants to hold the broken bone in its correct alignment until the bone is healed.Usually this is only required for the overall shape of the bone, though about 35% of fractures will enter the joint surface of the radius, which in my hands is best managed with an arthroscopic assisted reduction (see minimal additional surgical injury).

Usually, this means an operation to “reduce” or correct the shape and “stable fixation” to hold the correction. On an individual basis, this is most likely if we can return the skeleton to its normal shape and hold it there until it has healed. In most cases, my patients wish to attempt to return to as close to normal as possible. Rather than seeing if the patient can cope with a crooked skeleton, or at least doesn’t complain too much, I view my role as helping patients maximise their chances of returning to their desired level of function.

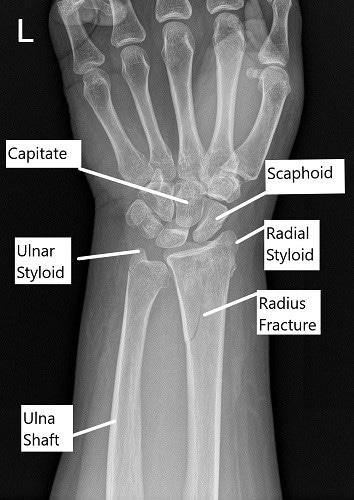
In active patients, a radius with an abnormal shape will often lead to mal-alignment of the upper and lower radio-ulna joints, which either restricts forearm motion or leads to abnormal motion (instability) of the lower joint. Much more common is that the fracture heals in an abnormal position. It is very rare for a fracture to not heal. The alignment and stability of the fracture fragments is very important in determining the outcome of the fracture, and whether surgery has a role in optimising the outcome. The path of the fracture line(s) may involve the wrist (radio-carpal) or lower (distal) radio-ulnar joints, in which case is it known as an intra-articular fracture. The pattern of the fracture can vary considerably. The radius is involved with four joints – at the elbow, the upper radio-ulnar joint, the lower radio-ulnar joint and the wrist (radio-carpal) joint (see figure).įractures of the lower (distal) radius are very common in all age groups. The radius is one of the two forearm bones which extend from the elbow to the wrist, the other is the ulna.


 0 kommentar(er)
0 kommentar(er)
